Treating tumors with engineered dendritic cells
Dendritic cells (DCs) work at the forefront of the immune system. They can actively capture antigens, such as fragments of viruses, bacteria, and mutated cancer cells, and direct other immune cells against those invading agents. This process, called antigen presentation, often results in the activation of a second type of immune cell, the CD8 T cell, which can eliminate infected or abnormally mutated cells. Thus, DCs play an important role in orchestrating immunity against pathogens and cancer cells.
Unfortunately, tumors often erect barriers against the body’s immune system, allowing them to grow uncontrolled. This setback, called immunosuppression, may involve the inhibition of DCs and their ability to present tumor antigens to CD8 T cells.
Addressing the limitations of traditional vaccines
Over the last few decades, researchers have worked to overcome tumor-induced immunosuppression by various strategies, collectively called immunotherapies, some of which are approved treatments effective in patients with certain cancers. One approach is to generate DCs from the blood monocytes (a type of immune white blood cells) of a patient with cancer, expose them in the laboratory to defined tumor-derived material from a tumor biopsy (antigen loading step), and then reintroduce them into the patient’s body. This procedure, often referred to as a DC vaccine, is expected to significantly enhance the presentation of tumor antigens to CD8 T cells.
However, DC vaccines have produced mixed results in clinical trials. One potential limitation is the use of monocyte-derived DCs. These cells lack certain essential properties of naturally occurring DCs, such as type I DCs (cDC1), which play a crucial role in activating CD8 T cells. Another potential shortcoming is its dependence on the antigen loading step, which uses predefined antigens that may not represent the full spectrum of relevant antigens present in cancer cells. Addressing the limitations of traditional DC vaccines could enhance their therapeutic efficacy.
A team of scientists led by Michele De Palma, associate professor in the School of Life Sciences and director of the Agora Cancer Research Center, has now developed engineered DCs with the capacity to differentiate into cDC1 and to stimulate anti-tumor immunity when transferred to mice with tumors, without the need for antigen loading step. The study is published in Nature Cancer.
“Our strategy does not use the monocyte-derived DCs employed in previous studies, but relies on a population of DC progenitors, called DCPs, which we can produce in vitro in the laboratory from readily available sources, such as blood and bone marrow”, De Palma explains.
Surpassing the outcomes
When engineered to express two immune-stimulatory molecules (IL-12 and FLT3L), the DCP could initiate effective anti-tumor immune responses in various cancer models, surpassing the outcomes achieved with other traditional DC formulations. “Remarkably, the engineered DCPs worked in the absence of antigen loading, which implies that they could be potentially effective against a broad range of human cancers, so irrespective of the antigens that they express”.
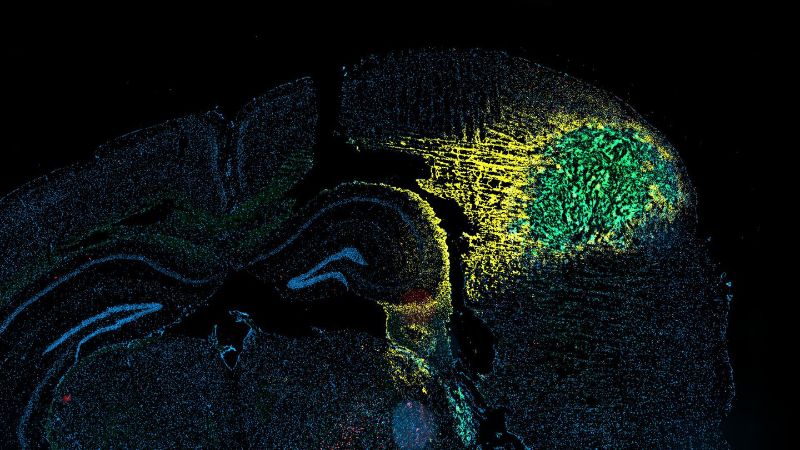
The ability of engineered DCPs to broadly engage multiple components of the immune system, not limited to CD8 T cells, may explain their effectiveness. “A very promising result was the ability of the DCPs to unlock the efficacy of CAR-T cells in eradicating brain tumors in mice”, says Professor Denis Migliorini, head of neuro-oncology at UNIGE and one of the study’s authors. CAR-T cells are another class of engineered immune cells already approved for the treatment of certain tumors, but their efficacy in brain cancer has so far been limited. “We are committed to combine DCPs with CAR-T cells in patients with incurable brain cancer”, adds Migliorini.
“Our preclinical results require further development and testing before moving to clinical application," cautions De Palma. DCPs can be readily obtained from human blood, which should facilitate the translation of preclinical results into a potentially transformative cancer immunotherapy.