Better choice of contraceptives can prevent breast cancer
Hormonal contraceptives, e.g. the pill, the patch, and the vaginal ring, contain synthetic hormones that prevent pregnancy by either stopping ovulation, changing the cervical mucus to stop sperm from passing through the cervix and finding an egg, or changing the womb’s lining to prevent a fertilized egg from being implanted in it.
Despite their widespread use, hormonal contraceptives are known to increase the risk of breast cancer, which is the most common cause of cancer-related death among women worldwide, and also topped the list of most commonly diagnosed cancers in 2020.
The main component of hormonal contraceptives are progestins, which, mimic the female sex hormone progesterone. Progesterone is involved in a number of biological processes, including the menstrual cycle, pregnancy, and various aspects of fetal development, like brain programming.
Now, a team of scientists led by Professor Cathrin Brisken at EPFL’s School of Life Sciences, have taken a thorough and close look at the different biological effects that different progestins in hormonal contraceptives have on the breast tissue – the mammary epithelium. The work is published in EMBO Molecular Medicine.
“Although we know how different contraceptive formulations affect the cardiovascular system, we know little about their effects on the breast,” says Brisken. “So we developed new approaches to compare the most commonly used progestins in different hormonal contraceptives and were surprised to find that some of them stimulate cell proliferation in the breast – while others do not.”
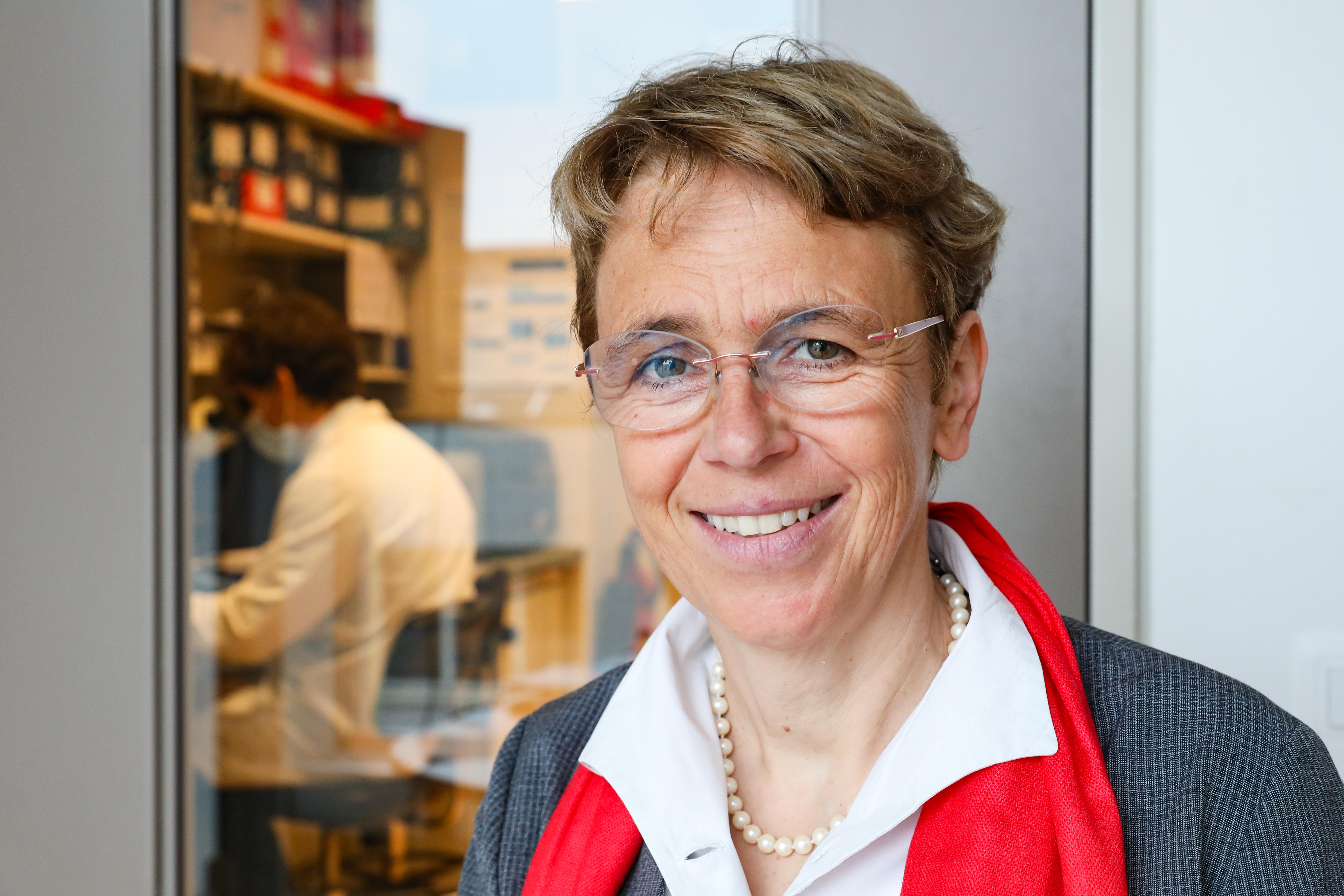
Cathrin Brisken © Alain Herzog / EPFL
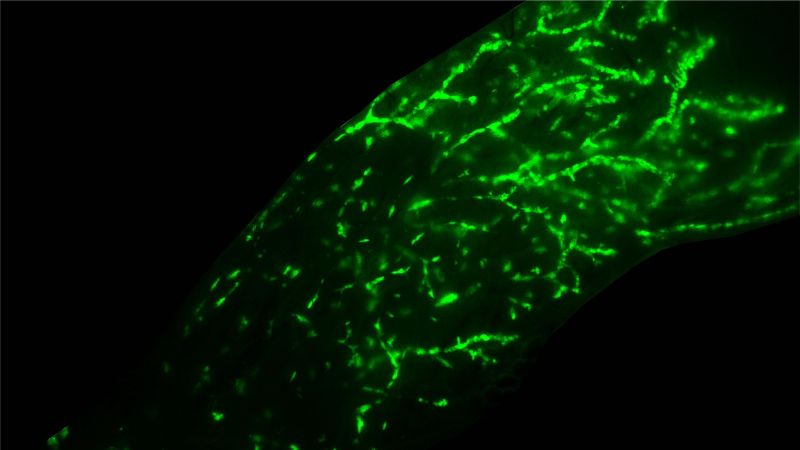
The researchers tested the effects of prolonged exposure to different progestins on human breast epithelial cells or HBECs, which line the inner layer of the breast. To do this, they developed “humanized” mouse mammary glands by grafting breast epithelial cells from donated human breast tissue from reduction mammoplasty samples into the animals’ milk ducts and monitoring their growth in vivo.
“We found that HBECs engraft and proliferate in mouse milk ducts, maintaining hormone receptor expression and hormone responsiveness, which are crucial factors for establishing a relevant preclinical model and thereby to foster translational research,” says Brisken.
The team realized that what distinguished the stimulatory and the innocuous progestins were their “androgenic properties” – a technical term for substances that trigger the development of male characteristics, such as body hair, muscle mass etc. This isn’t as strange as it sounds: progesterone, mostly known as a female hormone, is used for the production of the famous male hormone testosterone in both women and men.
Some progestins have androgenic properties, acting like testosterone; some actually block them. The key is a protein known as the androgen receptor, which, when activated by an androgenic progestin, travels into the cell’s nucleus where it regulates the expression of certain genes.
Working with the epithelial cells in a mouse model, the researchers found that androgenic progestins act through the androgen receptor to induce the expression of the protein Rankl, which plays an important role in cell proliferation in the mammary epithelium. This effect was not seen with anti-androgenic progestins.
The study showed that androgenic – but not anti-androgenic – progestins promote cell proliferation. “Exposing human breast epithelia to androgenic progestins for prolonged periods of time caused hyperproliferation and changes in the cells that are associated with early, pre-malignant lesions – at least in xenografted human breast epithelia,” says De Martino.
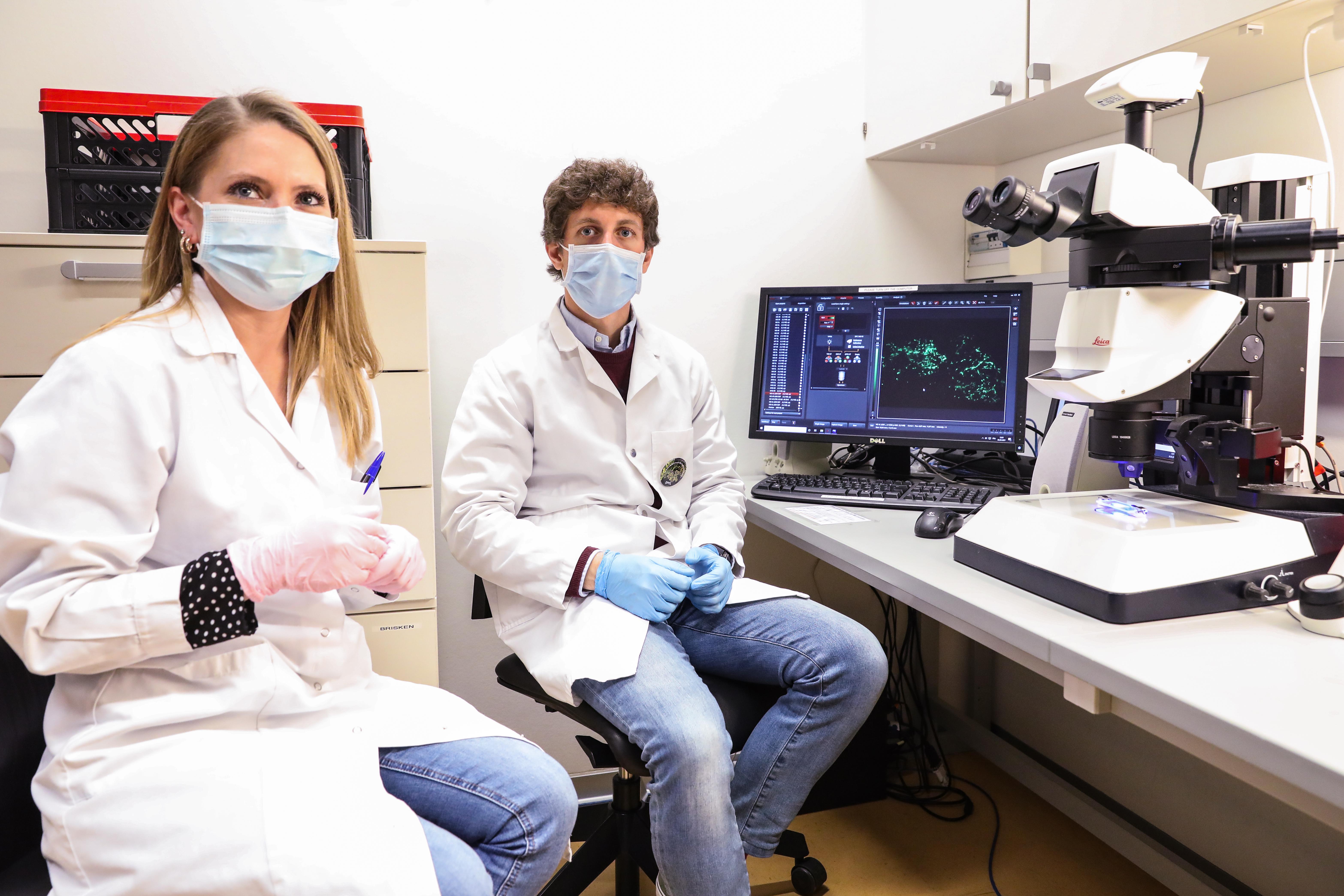
Laura Battista and Fabio de Martino © Alain Herzog / EPFL
“Hormonal contraception exposes women to different progestins with or without estrogen,” says Brisken. “The androgenic properties of progestins determine their biological activity in the breast epithelium, and reveal an unexpected role for androgen receptor activity in the proliferation of breast epithelial cells.”
The crucial insight of the study is that progestins with anti-androgenic activity may be a safer option with regards to breast cancer risk than testosterone-related compounds, e.g. the widely used contraceptive levonorgestrel (“Plan B”). “It might be possible to prevent breast cancer associated with contraception by making more informed choices taking the molecular composition of a contraceptive into account,” concludes Brisken.