A first for Switzerland: proton therapy to treat lung cancer
Lung cancer is the deadliest type of cancer in Switzerland and also one of the most common: it affects around 4,500 patients every year. Surgery is the most usual form of treatment. In advanced tumours, surgery is followed up with chemotherapy and radiotherapy, and sometimes immunotherapy as well. However, not all tumours can be surgically removed, so scientists are currently conducting intensive research into improving non-invasive treatment methods. For patients in Switzerland, the Paul Scherrer Institute PSI now offers a novel alternative: proton beam therapy (PBT). PSI researchers hope this will extend patient survival rates – even without surgery – and reduce secondary effects caused by radiotherapy, such as heart problems and pneumonitis.
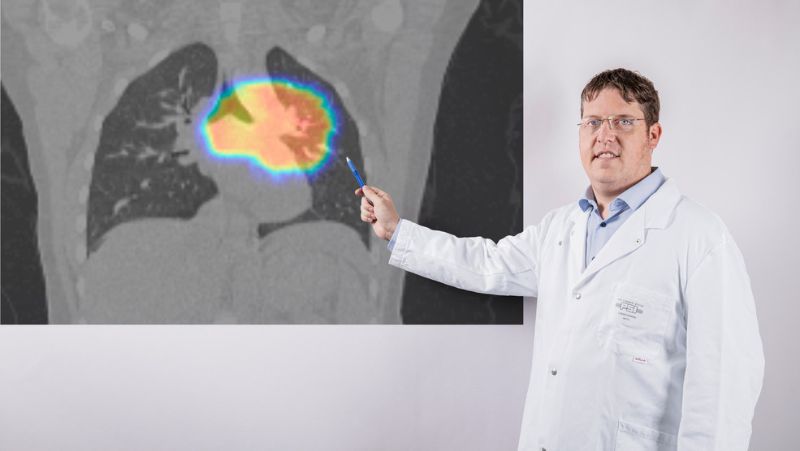
"Today we have used proton therapy, as part of an international Phase 3 clinical trial, to treat our first patient with lung cancer, specifically a non small cell bronchial carcinoma," says Damien Weber, Chief Physician and Head of the Center for Proton Therapy (CPT) at PSI. "The patient had an advanced stage tumour that could not be surgically removed." The study is led by the US research organisation overseeing oncologic clinical trials, NRG Oncology. PSI is taking part together with the Radio-Oncology Centre of the Cantonal Hospitals of Aarau (KSA) and Baden (KSB) – the only institutes outside the US to do so. The aim of the trial is to compare the outcomes of established radiotherapy with proton therapy in the treatment of non small cell bronchial carcinoma – the most common form of lung cancer – in the advanced, inoperable stage.
"The fact that our radio oncology team and PSI have been invited to take part in the trial is chiefly down to both institutions’ many years of expertise in the field of radiotherapy and our membership of NRG Oncology," says Oliver Riesterer, Chief Physician at the Radio-Oncology Centre KSA and KSB. "We can offer cancer patients a unique opportunity: to take part in Switzerland’s first randomised study comparing the outcomes of proton therapy and traditional radiotherapy." Patients are randomly allocated to either type of treatment: some receive proton therapy at PSI, others radiotherapy at the Radio-Oncology Centre KSA-KSB. "Since we have the most modern equipment currently available for conventional radiotherapy, we can compare the best with the best," says Riesterer in describing the study design.
A fine distinction
Both types of radiation damage the genetic material in the tumour cells and thus kill them – the difference is thought to lie in their physical properties: classical radiation therapy uses X-rays, or photons, whereas proton therapy dispenses charged particles. Nowadays, X-rays can be focused very precisely on the tumour, but the photons also spread into the surrounding healthy tissue and damage it – the higher the radiation dose, the greater the damage. By contrast, proton beams provide much higher precision. The spot scanning technique developed at PSI directs a beam of proton particles no thicker than a pencil onto the tumour and scans the entire tumour from back to front. The protons deposit almost their entire energy directly in the tumour, destroying the cancer cells. The healthy tissue in front of the tumour only receives a very low dose, and the tissue behind the tumour none at all, because the beam is slowed down by the tumour tissue (unlike photon therapy). The impact of the radiation on the healthy tissue is therefore much weaker.
"We expect proton therapy to be more effective purely by virtue of its physical properties," says Weber. The doctor recalls a young patient whom he already treated with proton therapy a few years ago at PSI on the basis of this assumption. "The outcomes were very good. So far, however, we have not been able to conclusively show whether all patients benefit from proton therapy . This is due to the lack of high-quality clinical trials that directly compare both methods." For such studies to provide meaningful results, patients must undergo a randomised trial where they are assigned either radiotherapy or proton therapy, as this is the only way of minimising the effect of other factors. However these randomised studies are very time-consuming and expensive. In oncology, they are therefore almost always performed in larger institutions with high quality standards and patient numbers.
Before the trial could even start, PSI – like all the study participants, including the Radio-Oncology Centre KSA-KSB – had to go through a lengthy process of accreditation by the M.D. Anderson Cancer Center in Houston, an institute commissioned by NRG Oncology. "For data comparison purposes, it is vital to ensure that all patients are treated in the same way and with the same quality standards," explains Dominic Leiser, radio oncologist at PSI. "So we had to prove, for example, that we can precisely target a tumour in a dummy patient within a tolerance of two millimetres and show that the dosage administered is exactly the one we calculated beforehand." To provide the required quality control, the PSI team performed radiotherapy on “phantoms”. These dummies have integrated devices for measuring doses and mimic the properties of a human patient – it is even possible to simulate the movement of the lungs while breathing.
A big step for proton therapy
The treatment of a cancer patient using this method opens a new chapter in proton therapy at PSI. While this type of therapy has already become established for treating certain tumours in the area of the head, neck and torso, the treatment of tumours in the lungs is new territory. As the lungs move when breathing, it is particularly difficult to direct proton beams at the lungs with a high degree of accuracy, as their position changes by up to two centimetres with every breath taken. "We need to make sure that the proton beam scans the entire tumour despite the breathing movement," Leiser explains. "We use a special trick for this, known as rescanning. The tumour and surrounding area are scanned several times with the proton beam. But this sometimes leads to more healthy lung tissue than necessary being affected." In order to avoid this, PSI scientists have a second trick: a dose of protons is only fired when the lungs breathe out. To achieve this, a computer tomogram (CT scan) is taken that records all the inhalation and exhalation phases. A marker roughly the size of a two-franc piece is placed on the patient’s chest which moves up and down while the patient is breathing and can be visualised on the CT scan. During the acutal proton radiation procedure, the position of this marker is then monitored by a special video camera. As soon as the marker shows that the patient has fully exhaled, a dose of protons is fired. Conversely, the proton beam is stopped while the patient breathes in. "This technique is very comfortable for patients, as it allows them to breathe quite normally during treatment," says Leiser.
The clinical trial is due to number 330 patients in total, with around 10 of them in Switzerland. "The cooperation of our two institutions is a milestone for cancer patients in the Canton of Aargau," says Weber. Both centres are keen to cooperate more closely also in other projects. Riesterer stresses: "Our goal is to use both photon and proton therapy to achieve the best possible outcomes for our patients."